- Products
- New Products
- Featured Products
- Color and Print Themes
- Blood Pressure Measurement
- NIBP / Vital Sign Monitors
- Digital Aneroid Sphygmomanometers
- Palm Aneroid Sphygmomanometers
- Pocket Aneroid Sphygmomanometers
- Pro's Combo Sphygmomanometers
- Multicuff Sphygmomanometers
- Clock Aneroid Sphygmomanometers
- Mercury Sphygmomanometers
- Home Blood Pressure Measurement
- Adcuff +
- Gauges
- Bulb & Valves
- Disposable Cuffs
- Reusable Cuffs & Bladders
- Sphygmomanometer Accessories
- Sphygmomanometer Parts
- Caseware
- CPR / Airway
- EENT
- Instruments & Accessories
- Laryngoscopes
- Penlights
- Pulse Oximeters
- Stethoscopes
- Thermometry
- Vital Signs Monitors
- Solutions
- About ADC
- Learning Center
- Support
- Blog
- Contact
How to Get an Accurate Temperature Measurement

Written By:
Marc Blitstein / President & CEO
Posted On:
February 12, 2019
Step 1: Purchase an ADC Adtemp™ thermometer.
Step 2: Remove from package.
Step 3: Follow included instructions for use.
If only it were that easy, right? Well, in some ways, it is. Accurate temperature measurements start with using the right brand of thermometer. Virtually all digital stick thermometers and most infrared thermometers (infrared includes both non-contact style and tympanic models, which read at the ear) are made in China and sold to domestic firms under dozens of brand names. But not all Chinese factories produce quality products and the majority of U.S. “importers” don’t have the facilities to test their devices.
ADC uses only ISO-certified subcontractors to produce our digital thermometers. We also have our own, in-house testing lab right here in our New York headquarters. This allows us to randomly test incoming shipments to make sure they comply with international standards for accuracy. For digital stick thermometers, accuracy is required to ± 0.2°F or 0.1°C (when tested on a water bath), within the range of 98°F and 102.0°F.
We’re actually one of the very few firms that does this kind of in-house testing, which is why the prestigious consulting firm Frost and Sullivan named our digital stick thermometry program best in the U.S. We’ve used that same lab equipment to test our competitors’ thermometers and found many didn’t meet accuracy requirements or measure temperature in the time specified, or they had expired batteries.
But how do you ensure you get accurate measurements with your thermometer, regardless of the brand? It helps to understand temperature measurement and the instrument’s limitations.
Let’s start with a bit about body temperature.
What Is Body Temperature?
Core temperature is the temperature deep within your body. Most think of normal temperature as 98.6°F, but that can be misleading. (And it might not even be “normal” anymore; several recent studies have suggested that human body temperatures have been dropping over the last century.) Like other vital signs, including blood pressure, this number merely represents a population average. At the individual level, everyone’s body temperature is unique and can vary by about a degree. So it’s likely your average body temperature falls more in the 97.6°F to 99.6°F range.
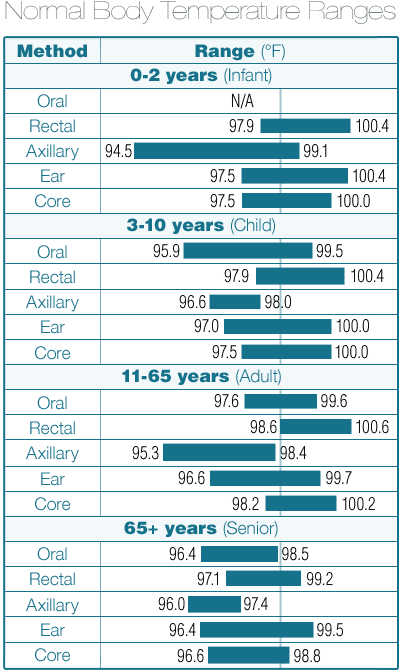
In addition, your body temperature varies, not just when you’re ill, but at different times of day and depending on certain environmental factors. Age also plays a role, as does site selection (where on your body you take the measurement). The chart included here shows how some of these variables impact temperature ranges.
If you take your temperature a few times when “healthy,” you can get a baseline of your normal temperature.
Where Is Temperature Measured on the Body?
There are three common sites for temperature measurement using stick thermometers – oral, rectal, and axillary (underarm) – and three for temperature measurement using an infrared device – inner ear, forehead, or temporal artery.
Stick thermometers report the actual temperature they detect. Infrared thermometers generally don’t. Instead they convert the observed reading to either a core or oral equivalent. Check with the manufacturer of the infrared thermometer to understand how their unit works.
Digital stick thermometers are offered in universal, oral, or rectal designs. Most use the exact same circuitry, though, and are simply color coded for control in institutional settings. (So a digital stick thermometer that’s coded for oral can in fact be used at all three sites with equally accurate results.)
True core body temperature is most closely represented by rectal temperature readings. Oral readings tend to be about 1°F cooler. Axillary are another 1°F cooler than that.
Some sites make it easier to obtain accurate readings. Rectal is the easiest because it provides excellent surface contact and less opportunity for faulty technique to influence readings. Oral is second easiest, and axillary the most challenging.
Measurement site also affects response time for most digital stick thermometers, again because of improved surface contact with the probe. Rectal measurements are faster than oral which are faster than axillary. A typical 60-second digital stick thermometer measures orally in about 60 seconds and rectally in about 45 seconds, while axillary measurement will take 75 to 90 seconds.
Digital Stick Technology
Why does response time vary? Because most stick thermometers use a technology referred to as “peak hold” (the other technology is “predictive”). Peak-hold thermometers display a reading when no further increase in temperature is observed. The circuitry is designed to obtain an accurate reading in about the time stated in the packaging or product spec. Peak hold are most commonly offered in 60-, 30-, and 18-second (oral) models; the faster the reading the more expensive.
Though typical digital stick thermometers measure orally in 60 seconds, some read in as little as two seconds. These faster units often use predictive technology, which displays readings in exactly the time indicated in their specification. To do that they predict the final reading using proprietary software.
Proper Oral Measurement Technique
Since oral is by far and away the most popular measurement site, let's chat a bit about the proper technique. First, it’s important that the patient’s oral temperature is stabilized. If they just came in from cold weather, or had a sip of hot coffee or cold soda, wait a few minutes before taking the measurement.
The probe tip should be seated under the tongue in the sublingual pocket, which is where the back of the tongue and floor of the mouth meet. The patient’s mouth should be relaxed. Clamping elevates temperature and risks damage to the thermometer. Even though thermometers today are generally very light, we recommend holding it in place with the hand (either the patient’s or the practitioner’s). That reduces the risk of biting the thermometer or letting it slip from position. Patients shouldn’t talk during measurement.
Unexpected Measurements
What if you get a bad reading? Try another measurement. In all likelihood, the probe wasn’t seated properly or the patient’s mouth wasn’t given the chance to stabilize. If you get a second reading that doesn’t appear right but was consistent with the previous reading, it probably is correct.
And remember, you’re generally looking for meaningful variances from a temperature baseline. A temperature of 99.2°F taken rectally is probably not an issue for most patients. For an oral reading, it’s marginal. Most physicians are concerned when oral temperature exceeds 99.9°F and rectal exceeds 99.5°F to 100.9°F.
While we don’t get too many thermometers back with complaints about accuracy, we do get a few. And to date, we have never found one that failed our accuracy tests. Never. In all likelihood, the measurement technique was flawed or the patient’s temperature wasn’t what you expected, causing the incorrect conclusion that there was a problem with the device.
